If you need to print this PDF or save for later
click below to download your copy.
[button size=”medium” style=”secondary” text=”Download PDF” link=”https://vetovationnew.instawp.xyz/wp-content/uploads/2016/01/ovariectomy-vs-ovariohysterectomy-copy.pdf” target=”none”]
Making a Rational Choice Between Ovariectomy and Ovariohysterectomy in the Dog: A Discussion of the Benefits of Either Technique
BART VAN GOETHEM, DVM, AUKE SCHAEFERS-OKKENS, DVM, PhD, Diplomate ECAR, and JOLLE KIRPENSTEIJN, DVM, PhD, Diplomate ACVS & ECVS
Objective—To determine if ovariectomy (OVE) is a safe alternative to ovariohysterectomy (OVH) for canine gonadectomy.
Study Design—Literature review.
Methods—An on-line bibliographic search in MEDLINE and PubMed was performed in December 2004, covering the period 1969–2004. Relevant studies were compared and evaluated with regard to study design, surgical technique, and both short-term and long-term follow-up.
Conclusions—OVH is technically more complicated, time consuming, and is probably associated with greater morbidity (larger incision, more intraoperative trauma, increased discomfort) compared with OVE. No significant differences between techniques were observed for incidence of longterm urogenital problems, including endometritis/pyometra and urinary incontinence, making OVE the preferred method of gonadectomy in the healthy bitch.
Clinical Relevance—Canine OVE can replace OVH as the procedure of choice for routine neutering of healthy female dogs.
© Copyright 2006 by The American College of Veterinary Surgeons
INTRODUCTION
GONADECTOMY is one of the most frequently performed surgical techniques in veterinary practice because it is the most reliable means of pet population control.¹ The importance of pet population control is underscored by the American Humane Association’s Animal Shelter Reporting Study that between 3.9 and 5.9 million dogs are euthanatized annually in the United States.²
Gonadectomy can be performed by ovariectomy (OVE) or ovariohysterectomy (OVH), the latter being the preferred approach in the United States.³⁻⁵ This preference is most likely based on the presumption that future uterine pathology is prevented by removing the uterus. In The Netherlands and some other European countries, OVE is routinely performed and has replaced OVH as the standard approach for gonadectomy; the uterus is only removed when uterine pathology is present. Despite longterm studies that compare risks and complications associated with these techniques, and favor OVE as the preferred technique, OVE is not generally accepted in the United States.⁶⁻⁹
Our aim was to evaluate and report possible differences in surgical complications between OVE and OVH. We reviewed the veterinary literature for evidence that would identify whether either technique could be considered superior for routine neutering of dogs.
SURGICAL TECHNIQUE
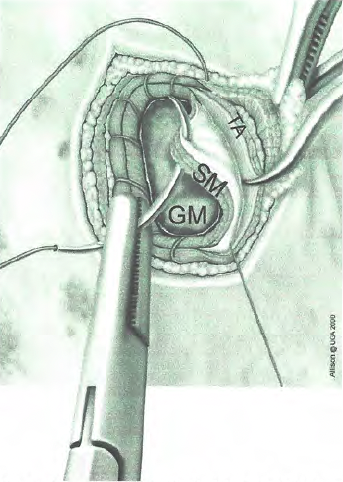
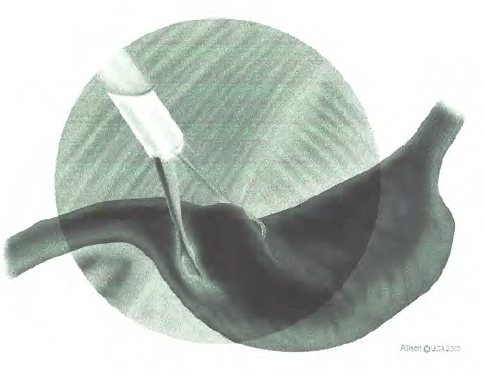
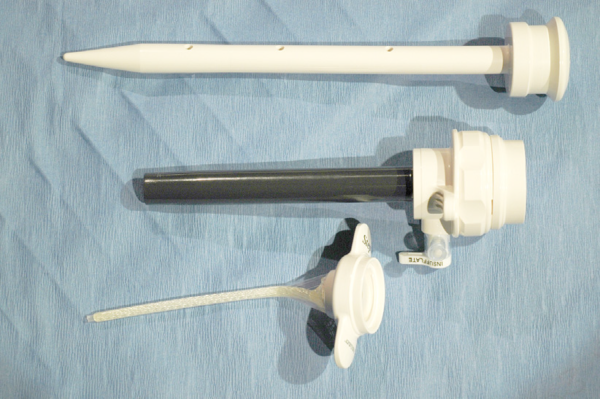
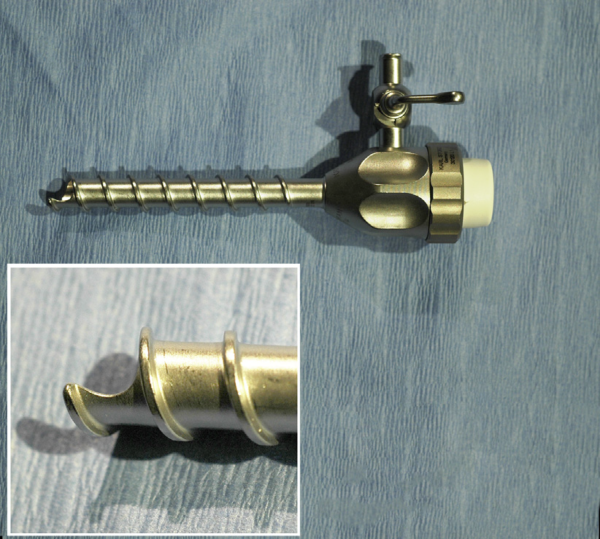
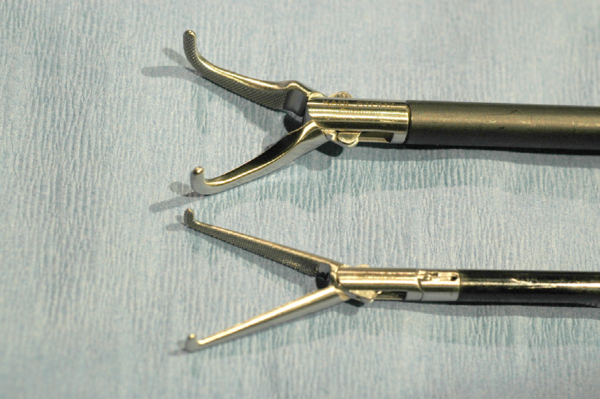
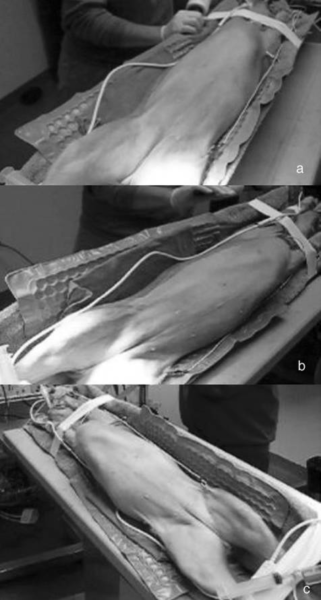
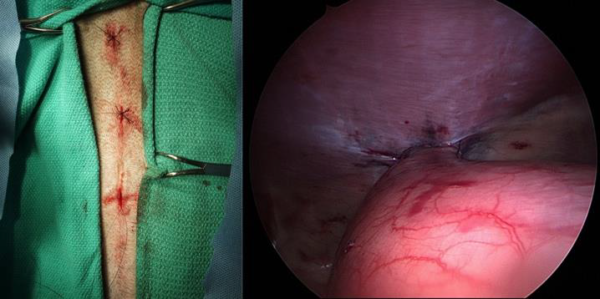
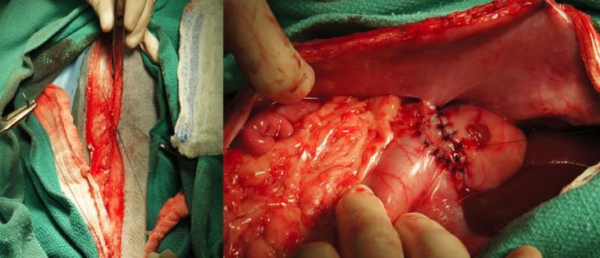
OVE is started by a median celiotomy extending from the umbilicus to approximately halfway between umbilicus and os pubis, depending on dog size. In deep-chested or obese dogs, it is sometimes necessary to enlarge the incision cranially to allow sufficient exposure of the ovarian pedicle.⁴,¹⁰ The ovary was located, and retracted caudally to expose the suspensory ligament and ovarian pedicle. The suspensory ligament was stretched, broken, or transected by electrocoagulation or scissors, to improve manipulation and observation of the pedicle. The arteriovenous complex within the pedicle, arising from the ovarian artery and vein was ligated with 0-4/0 absorbable suture material, depending on pedicle size, after which it was transected. The uterine artery and vein were ligated at the cranial tip of the uterine horn, 5 mm caudal to the proper ligament, using 2/0-4/0 absorbable suture material, and transected at the proper ligament.¹¹ After excision, the ovarian bursa was opened and the ovary inspected to confirm complete ovarian removal.³,¹¹
OVH was also performed through a median celiotomy, although, based on the dog’s size and body condition, the incision was lengthened in a caudal direction. After the ovarian pedicles were ligated and severed, the broad ligament was examined. If it is vascular, it is ligated with 1 or 2 ligatures using 2/0-4/0 absorbable suture material before it is cut or torn. A clamp was placed on the uterine body just cranial to, or on, the cervix. The uterine arteries were individually ligated proximal to the clamp using 2/0-4/0 absorbable suture material and the uterus, was ligated circumferentially in the crushing groove that remains after removal of the clamp using 0-4/0 absorbable suture material. After inspection for potential bleeding at the ligated pedicles, the celiotomy was closed in layers.³,⁴,¹¹⁻¹³
From a technical perspective, OVE is a minimally invasive veterinary surgery and less time-consuming than OVH. Although it is possible to perform OVH through a small median celiotomy, atraumatic technique and correct placement of the uterine ligature near the cervix typically requires a larger celiotomy compared with OVE. Thus, the duration of surgery and anesthesia should be shorter for OVE, and because the celiotomy is shorter, the broad ligaments are not disrupted, and the uterine stump left intact, there should also be less surgical trauma resulting from the minimally invasive veterinary surgery.
INDICATIONS FOR OVE AND OVH
OVE, also known as laparoscopic spay, is the most commonly performed for elective neutering; however, it is also indicated for treatment of ovarian tumors, to promote involution of placental sites (non-responsive to medical treatment), to prevent recurrence of vaginal hyperplasia, to prevent hormonal changes that can interfere with medical therapy in patients with endocrine diseases (e.g., diabetes), and to eliminate the transfer of inherited diseases (e.g., generalized demodicosis).³,¹¹,¹⁴ OVE is also performed in young dogs ( ! 2.5 years) to decrease the incidence of mammary gland tumors. The relative risk for developing mammary gland tumors decreases when neutering is performed before first estrus (0.5%), between first and second estrus (8%), and between second estrus and 2.5 years of age (26%).¹⁵ Despite one contrary opinion,¹⁶ there is seemingly no benefit in performing OVH at the time of mammary tumor removal because neither tumor-related nor overall survival improve after OVH.¹⁷⁻¹⁹
OVH is the preferred laparoscopic spay treatment for most uterine diseases, including: congenital anomalies, pyometra, localized or diffuse cystic endometrial hyperplasia (CEH), uterine torsion, uterine prolapse, uterine rupture, and uterine neoplasia.³,⁴,¹¹,²⁰ In a study of 1712 canine OVHs, 1409 (82%) were performed for elective sterilization, and only 313 (18%) for reproductive tract disease (as adjunctive therapy for mammary neoplasia, for treatment of pyometra, endometrial hyperplasia, vaginitis, and several miscellaneous genital tract diseases).²¹ This and other reports clearly reflect textbook recommendations that the preferred technique for gonadectomy in dogs and cats is OVH.³⁻⁵,¹¹
SURGERY RELATED COMPLICATIONS
The primary rationale for selection of OVH or OVE is likely related to the expected frequency of short-term and long-term complications. In a retrospective study of 62 dogs that had OVH, 17.7% developed complications.22 Complications associated with OVE would be expected to be similar to those associated with the OVE component of OVH; however, other complications associated with removal of the uterus in OVH would not be expected with OVE. A review of reported complications after OVE and OVH is presented below (Table 1) and a logical decision for technique is suggested.
Intraabdominal Hemorrhage
Hemorrhage was the most common complication (79%) in dogs 425 kg in a review of 853 OVHs.¹⁰ Concurrently, hemorrhage has been determined to be the most common cause of death after OVH in large breed dogs.⁵,²⁰ Clinically important hemorrhage primarily occurs from the ovarian pedicles, the uterine vessels, or the uterine wall when ligatures are improperly placed,²³ and rarely occurs from vessels that accompany the suspensory ligament or within the broad ligament.⁴ Thus, comparing OVE with OVH, the likelihood of clinically important hemorrhage from the ovarian pedicles should be similar.
[table id=10 /]
Theoretically, OVH has additional risk for hemorrhage from vessels in the broad ligament and from uterine vessels near the cervix (where the uterine arteries are larger than at the tip of the uterine horn and bleeding can be more severe in comparison). Hemorrhage from uterine vessel rupture caused by excessive traction on the uterine body during OVH has been reported.²³
Vaginal Bleeding
Single nonabsorbable multifilament ligatures around the uterine body can predispose to erosion of uterine vessels, resulting in intermittent vaginal bleeding. Pearson reported vaginal bleeding in 11 (15%) of 72 dogs, 4–16 days after surgery.²³ Vaginal tamponade or exploratory celiotomy may be indicated, if the bleeding becomes severe. Vaginal hemorrhage may also be associated with infection caused by contamination during surgery, use of infected suture material, or from transfixation ligatures that enter the lumen of the uterus or cervix.²³
The advantage of ligating the uterine vessels at the uterine horn tip and transection at the proper ligament is that the uterine horn is not opened and the serosa remains intact. Bleeding from the vulva in the first week after surgery cannot occur. The only case in which one of the authors have observed a dog with vaginal bleeding after OVE was when the surgeon transected the uterine horn (and thus opened the lumen).
Ligation of the Ureter
Direct obstruction of a ureter occurs when the ureter is accidentally included in a ligature. For instance, if the pedicle is ligated too close to its base at the abdominal wall, because of inadequate exposure of the caudal pole of the kidney, the proximal aspect of the ureter may be incorporated.²⁰ More often the distal part of the ureter is involved because of its close location to the uterine body. Inadvertent, suture-associated occlusion of the distal ureter is more common if a distended urinary bladder displaces the trigone cranially.²⁰ Okkens et al⁸ reported complications after OVH in 109 dogs, admitted over a 2-year-period (1977–1979) at the University of Utrecht, The Netherlands. Among these dogs, 18 had signs related to the urinary system. Direct ligation of the ureter was observed at the ovarian pedicle in 2 dogs (11%) and at the distal ureter by uterine ligature in 3 dogs (17%). It is evident that the chance of ligation of the proximal ureter during OVE is identical to the OVH technique, but distal ureteral ligation is nonexistent during OVE.
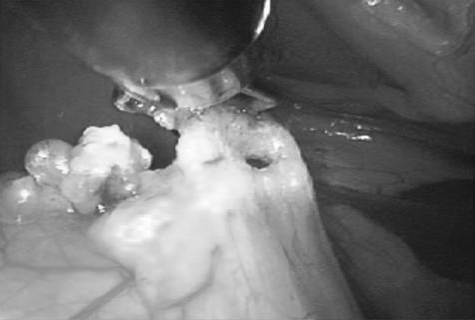
Ovarian Remnant Syndrome
Recurrent estrus occurs after OVE or OVH when the ovaries are incompletely removed and residual ovarian tissue becomes functional. Collateral circulation to the ovarian tissue can develop even though the ovarian arteriovenous complex has been ligated and interrupted.³ In dogs, neither ectopic ovaries (ovarian tissue in an abnormal location such as in the mesentery), nor accessory ovarian tissue extending into the ligament of the ovary have been reported, in contrast to their occurrence in cats, cows, and humans.⁵,²⁴
Pearson²³ described 12 dogs with recurrent estrus in a group of 72 dogs with complications after OVH (17%). Okkens et al⁹ reported 109 dogs with complications after OVH, of which 55 dogs had complications of a gynecologic nature; residual ovarian tissue was observed in 47 dogs (43%). Of these dogs, 16 had bilateral, 25 rightsided, and 6 left-sided residual ovarian tissue. Ovarian remnants tend to be more commonly located on the right side. This higher frequency of right-sided ovarian remnants has been observed by others and is likely explained by a more cranial and deeper anatomic location of the right ovary, decreasing the ease of observation and removal.²³,²⁵ When performing OVE, the surgeon is placing 2 cuts close to the ovary (ovarian pedicle and proper ligament). One could argue, but this remains speculative, that there is an increased chance for ovarian remnants with OVE in comparison with OVH (where only 1 cut is made close to the ovary); however, this cannot be confirmed by literature review.
Most ovarian remnants occur after OVH.⁸,⁹,²³⁻²⁵ This may be because OVH is more commonly performed technique or because the celiotomy for OVH is located more caudally making observation of the (right) ovary more difficult. Decreased visualization enhances the chance for incorrect technique and the chance for ovarian remnants.10 In OVE, the incision can be positioned more cranial, avoiding this problem. Ovarian remnant syndrome can be avoided by correct surgical technique regardless of technique used. It is essential to have the incision cranial enough to allow complete visualization, especially of the right ovary. To achieve this with OVH a larger incision is necessary than for OVE.
Stump Granuloma
Inflammation and granuloma formation can be caused by ligatures of nonabsorbable suture material, poor aseptic technique, or excessive residual devitalized tissue (at the uterine body). Braided nonabsorbable suture materials, such as silk, nylon, or linen, and nonsurgical selflocking nylon bands (cable ties) have been implicated in most patients.²⁶ Okkens et al⁸ reported granulomas at the ovarian pedicle in 1 patient (6%) and at the uterine stump in 5 patients (28%). In dogs with gynecologic complications after OVH, Okkens et al⁹ observed 8 (15%) stump granuloma. The likelihood for development of a granuloma at the ovarian stump is not influenced by technique (OVE versus OVH), but the incidence of the more common granuloma at the uterine stump cannot occur with OVE. Granulomas at the uterine horn tip are possible, but to our knowledge, have not been described.
Fistulous tracts extending from the ligated ovarian pedicle can develop from inflammatory reaction to ligature material, primarily with braided nonabsorbable suture material. Ovarian pedicle granulomas were associated with sublumbar sinuses.²⁰ Pearson described 72 dogs with complications resulting from OVH at a time when nonabsorbable ligatures were routinely used, and reported 37 dogs with stump granuloma, of which 27 had sinus formation (38%).²³ In a report of 20 OVH-related fistulous tracts, the origin of the tract was unilaterally from an ovarian ligature in 12 animals and from the uterine ligature in 4 animals.⁵ Suture-associated fistulous tracts can easily be prevented by use of synthetic absorbable suture materials and surgical approach (OVE, OVH) should have no influence on occurrence of fistulous tracts.²⁶
Both OVE and OVH can result in fistulous tract formation from the ovarian stump. OVE technique might lead to formation of stump fistulas at the uterine horn tip; whereas, OVH technique has the additional risk for development of uterine stump fistulas. Both the uterine horn tip granuloma and the uterine horn tip fistula, however, can be prevented when correct OVE technique is used. Using correct technique, the uterine horn is not opened because transection is performed at the level of the proper ligament.
Miscellaneous
Many incidental complications after gonadectomy techniques including trauma to intestines or spleen, colonic incarceration,²³,²⁷ failure to remove gauze sponges from the abdomen before closure, endocrine alopecia, juvenile vulva formation, behavioral change, and eunuchoid syndrome have been reported.⁵ It seems unlikely that either technique will significantly increase the risk for any of these complications. Because OVE results in a smaller incision, complications such as incisional swelling, seroma, infection, dehiscence, delayed healing, ventral body wall dehiscence, self-inflicted trauma, and pain are expected to be less.
[table id=11 /]
LONG-TERM COMPLICATIONS AND UTERINE PATHOLOGY
When considering changing the routine neutering procedure from OVH to OVE, the importance of future complications and uterine pathology needs to be considered (Table 2). In particular, development of endometritis/pyometra, occurrence of neoplastic uterine changes, incontinence, and obesity should be considered.
Endometritis and Pyometra
Epidemiologic data for ~200,000 dogs covered by insurance in Sweden revealed that ~1800 nonspayed bitches were treated for pyometra in 1996. The risk of an intact bitch developing pyometra before 10 years of age was 23–24%.²⁸ Other studies, albeit on a smaller scale, had similar findings. Fukuda²⁹ reported a 15.2% chance for the development of pyometra in female dogs>4 years (n = 165) and Von Berky³⁰ reported a 14.9% chance for uterine disease (n = 175).
Thus, it is important to determine whether the uterus in ovariectomized dogs is predisposed to develop endometritis and pyometra. Pyometra has been defined as a hormonally mediated diestral disorder resulting from bacterial interaction with an abnormal uterine endometrial that has undergone pathologic changes assumed to be caused by an exaggerated response to progesterone stimulation.³¹ Recently, the concept of considering CEH– pyometra as a complex has been questioned. It has been suggested that 2 different disorders: one where CEH–endometritis appears to have a strong hormonal component and the other where pyometra might be more influenced by the bacterial component.²⁸ Nevertheless, both conditions are exclusively encountered in the luteal phase of the estrus cycle. Experimentally CEH or CEH–endometritis can be induced by administration of progesterone, even in ovariectomized bitches.²⁰ Withdrawal of progesterone treatment causes regression of the naturally occurring disease. Thus exposure to progestagen appears to be necessary for the development of CEH–endometritis.
A study by Okkens et al comparing the long-term effects of OVE versus OVH was conducted at the University of Utrecht in 1997.⁶ Questionnaires were sent to 264 owners of bitches that had either OVE (n = 126) or OVH (n = 138) performed for routine neutering 8–11 years earlier. Complete data were obtained for 69 OVE bitches and 66 OVH bitches. None of the OVE bitches had signs consistent with having had endometritis. With the exception of urinary incontinence, no other problems related to surgical neutering were identified. These findings agree with those of Janssens who performed OVE on 72 bitches and after a 6–10 year follow-up, no pyometra was detected.⁷ When OVE is correctly performed (all ovarian tissue removed), and in the absence of supplementation of exogenous progestagens, endometritis (CEH or pyometra) cannot occur.
Stump pyometra is uniquely associated with OVH, and can develop if endometrial tissue at the uterine stump is stimulated by either endogenous, because of incomplete ovarian tissue removal, or by exogenously administered progesterone.²⁰ In Okkens et al⁹ report on 55 dogs with gynecologic complications after OVH, 19 (35%) had stump pyometra associated with residual ovarian tissue. In the same study 47 bitches had histologically confirmed CEH–endometritis during celiotomy; abdominal exploration revealed the presence of residual ovarian tissue in all of these dogs. Another 7 dogs an enlarged and inflamed uterine stump, where no residual ovarian tissue was detected and on histology the inflammation was caused by an unabsorbed ligature (stump granuloma) without signs of CEH.⁹
These studies strongly suggest that progesterone is an essential factor in the occurrence of CEH–endometritis– pyometra and that correctly performed, OVH or OVE will prevent development CEH–pyometra in later life. OVE will not increase the chance for development of CEH–pyometra compared with OVH.
Uterine Tumor Formation
Uterine tumors are rare in the dog, with a reported rate of 0.4% of all canine tumours.³² The University of Pennsylvania Veterinary Hospital examined 33,570 female dogs between 1952 and 1966, and 96 gynecologic neoplasms (uterus, n = 11; vagina or vulva, n = 85) were detected in 90 dogs (0.27%).³³ This brings the overall chance for a uterine tumor to 0.03% (11/33570). Middleaged-to-older animals were most commonly affected and most canine uterine tumors were mesenchymal in origin. Of the uterine tumors, 85–90% were benign leiomyomas and 10% leiomyosarcomas. The true risk for development of malignant tumoral disease of the uterus is 0.003%. The prognosis associated with leiomyomas and other benign tumors is excellent because surgery is nearly always curative. For leiomyosarcomas and other malignant tumors, the prognosis remains good if there is no evidence of metastatic disease at surgery and complete excision is possible.³²,³⁴,³⁵ When performing gonadectomy, the surgeon has to balance the risk for possible tumoral development in the uterus when performing OVE, against the increase in surgery related complications when performing OVH.
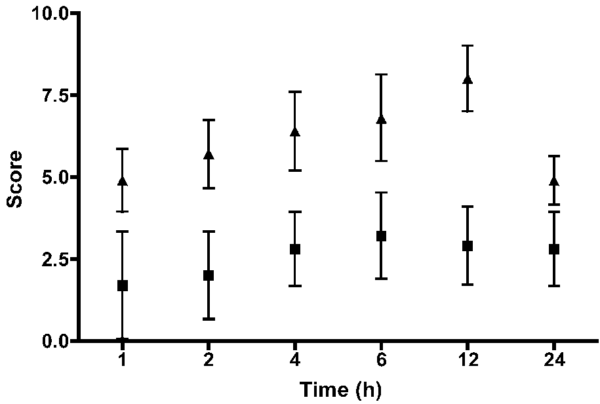
Urinary Sphincter Mechanism Incontinence
Adhesions or granulomas of the uterine stump that interfere with urinary bladder sphincter function or development of a ureterovaginal fistula can occasionally cause incontinence. The most common cause of incontinence in spayed dogs, however, is urethral sphincter mechanism incompetence (USMI), an uncommon disease in intact bitches with reported incidences of 0.2% (10/ 5315)³⁶ to 0.3% (7/2434).²⁰ Because of the underlying hormonal cause, a significant increase of this pathology in spayed bitches has been hypothesized.³⁷,³⁸ Nickel et al³⁹ reported a significantly impaired urethral sphincter mechanism in gonadectomized dogs. In a retrospective investigation, Holt and Thrusfield³⁶ using data from a general and a referral practice in UK, reported that 3% (53/1681) and 17.7% (296/1681), respectively, of dogs were considered incontinent after OVH. In Switzerland, up to 20% (83/412) of spayed bitches developed signs suggestive of urinary incontinence postoperatively.³⁸ Confounding factors in the development of incontinence include time of OVH, body weight, breed of dogs and tail-docking.⁵,³⁶,⁴⁰⁻⁴³ An increased risk in tail-docked bitches has been documented raising the incidence to 1.3 (34/2614) compared with 0.7% (29/4382) for undocked dogs.³⁶
Long-term studies have been unable to detect a difference between occurrence of incontinence in dogs after OVE compared with OVH. One of the initial reports concluded that there was no difference between OVE and OVH.⁴⁴ Another study reported that 54 of 260 OVE dogs developed incontinence (20.8%) compared with 29 of 152 OVH dogs (19.1%); however, this difference was not significant.⁴⁵ Okkens et al⁶ reported urinary incontinence in 15 dogs (11%) after long-term follow-up but no significant difference in incidence between OVE and OVH neutered bitches.
Body Weight Gain
Gonadectomy adversely affects the ability to regulate food intake and thus predisposes these animals to obesity.²⁰,⁴⁶ Inactivity and increased food intake contributes to weight gains up to 38%. Edney and Smith⁴⁷ observed that 21.4% of all dogs were overweight and spayed females were twice as likely to be obese compared with intact bitches. In another study, where dogs were exercised regularly and their food intake was controlled, there was no significant increase in weight in either spayed or intact females.⁴⁸ No significant difference in weight gain has been observed between dogs that had OVE versus OVH in other studies.⁴⁹,⁵⁰
CONCLUSION
The absence of randomized studies comparing complications after OVE and OVH in dogs forces us to interpret historical reviews of both techniques. The rational conclusion after review, when immediate postoperative complications are considered, is that either technique can be used for canine female gonadectomy. The surgeon has to choose the least invasive, fastest, and safest procedure. A major advantage of OVE is that it can be performed through a smaller celiotomy and with less traction on the female genital tract. Technically, OVH is more complicated (more tissue is ligated and transected), time consuming (because a larger celiotomy is needed to expose the entire uterus) and is therefore expected to be associated with a greater short-term morbidity when compared with OVE. However, differences in short-term postoperative morbidity between the 2 techniques have not been published. Increased risk for surgery-related complications associated with OVH are estimated for: intraabdominal and vaginal bleeding (because of larger vessel diameter near the uterine body), ureteral ligation (because of close proximity of the distal part of the ureter to the uterine body), ovarian remnants (because of the more caudally located incision), uterine stump complications, and sinus tracts (because of mucosal exposure).
Since 1981, after introduction of OVE, a minimally invasive veterinary surgery, as a standard technique for canine neutering at Utrecht University, no increase in short-term complications has been observed. With respect to long-term urogenital problems, including endometritis/pyometra and urinary incontinence, it has been clearly established that they do not occur more frequently with either technique. The overall chance for development of malignant uterine tumors is very low (0.003%), and, in our opinion, does not warrant performing a potentially more traumatizing surgical procedure, OVH, that might be associated with more postoperative complications.
Without benefit of more prospective studies comparing surgical complications between OVE and OVH, most evidence extracted from the literature leads us to the conclusion that there is no benefit and thus no indication for removing the uterus during routine neutering in healthy bitches. Thus we believe that OVE should be the procedure of choice for canine gonadectomy.
REFERENCES
1. Stockner PK: The economics of spaying and neutering: market forces and owners’ values affecting pet population control. J Am Vet Med Assoc 198:1180–1182, 1991
2. Nassar R: Pet population dynamics and community planning for animal welfare and animal control. J Am Vet Med Assoc 198:1160–1164, 1991
3. Fingland RB: Ovariohysterectomy, in Bojrab MJ (eds): Current Techniques in Small Animal Surgery (ed 4). Baltimore, MD, Williams & Wilkins, 1998, pp 489–496
4. Hedlund CS: Surgery of the reproductive and genital systems, in Fossum TW (eds): Small Animal Surgery (ed 1). St Louis, MO, Mosby-Year Book Inc, 1997, pp 523–524, 536– 537
5. Stone AE, Cantrell CG, Sharp NJ: Ovary and uterus, in Slatter D (eds): Textbook of Small Animal Surgery (ed 2). Philadelphia, PA, Saunders, 1993, pp 1293–1308
6. Okkens AC, Kooistra HS, Nickel RF: Comparison of longterm effects of ovariectomy versus ovariohysterectomy in bitches. J Reprod Fertil 51(Suppl): 227–231, 1997
7. Janssens LA, Janssens GH: Bilateral flank ovariectomy in the dog – surgical technique and sequelae in 72 animals. J Small Anim Pract 32:249–252, 1991
8. Okkens AC, van de Gaag I, Biewenga WJ, et al: Urological complications following ovariohysterectomy in dogs. Tijdschr Diergeneeskd 106:1189–1198, 1981
9. Okkens AC, Dieleman SJ, van de Gaag I: Gynaecologische complicaties na ovariohysterectomy bij de hond ten gevolge van: 1. het incompleet verwijderen van de ovaria en 2. een ontsteking van de uterus-cervix stomp. Tijdschr Diergeneeskd 106:1142–1158, 1981
10. Berzon JL: Complications of elective ovariohysterectomies in the dog and the cat at a teaching institution: clinical review of 853 cases. Vet Surg 8:89–91, 1979
11. Stone AE: Ovary and uterus, in Slatter D (eds): Textbook of Small Animal Surgery (ed 3). Philadelphia, PA, Saunders, 2003, pp 1495–1499
12. van Sluijs FJ: Ovariohysterectomy, in van Sluijs FJ (eds): Atlas of Small Animal Surgery. Utrecht, The Netherlands, Wetenschappelijke uitgeverij Bunge, 1992, pp 82–84
13. Toombs JP, Clarke KM: Basic operative techniques, in Slatter D (eds): Textbook of Small Animal Surgery (ed 3). Philadelphia, PA, Saunders, 2003, pp 208–212
14. Wheeler SL, Magne ML, Kaufmann J: Postpartum disorders in the bitch: a Review. Compend Contin Educ Pract Vet 6:493, 1984
15. Schneider R, Dorn CR, Taylor DO: Factors influencing canine mammary cancer development and postsurgical survival. J Natl Cancer Inst 43:1249–1261, 1969
16. Sorenmo KU, Shofer FS: Goldschmidt: effect of spaying and timing of spaying on survival of dogs with mammary carcinoma. J Vet Intern Med 14:266–270, 2000
17. Philibert JC, Snyder PW, Glickman N, et al: Influence of host factors on survival in dogs with malignant mammary gland tumors. J Vet Intern Med 17:102–106, 2003
18. Morris JS, Dobson JM, Bostock DE, et al: Effect of ovariohysterectomy in bitches with mammary neoplasms. Vet Rec 142:656–658, 1998
19. Yamagami T, Kobayashi T, Takahashi K, et al: Prognosis for canine malignant mammary tumors based on TNM and histologic classification. J Vet Med Sci 58:1079–1083, 1996
20. Kyles AE, Aronsohn M, Stone EA, et al: Urogenital surgery, in Lipowitz AJ, et al. (eds): Complications in Small Animal Surgery. Baltimore, MD, Williams & Wilkins, 1996, pp 496–503
21. Wilson GP, Hayes HM: Ovariohysterectomy in the dog and cat, in Bojrab MJ (eds): Current techniques in small animal surgery (ed 2). Philadelphia, PA, Lea & Febinger, 1983, pp 334–338
22. Pollari FL, Bonnett BN, Bamsey SC, et al: Postoperative complications of elective surgeries in dogs and cats determined by examining electronic and paper medical records. J Am Vet Med Assoc 208:1882, 1996
23. Pearson H: The complications of ovariohysterectomy in the bitch. J Small Anim Pract 14:257–266, 1973
24. Miller DM: Ovarian remnant syndrome in dogs and cats: 46 cases (1988–1992). J Vet Diagn Invest 7:572–574, 1995
25. Wallace MS: The ovarian remnant syndrome in the bitch and the queen. Vet Clin North Am Small Anim Pract 21:501– 507, 1991
26. Werner RE, Straughan AJ, Vezin D: Nylon cable band reactions in ovariohysterectomized bitches. J Am Vet Med Assoc 200:64–66, 1992
27. Coolman BR, Maretta SM, Dudley MB, et al: Partial colonic obstruction following ovariohysterectomy: a report of three cases. J Am Anim Hosp Assoc 35:169–172, 1999
28. Fransson BA, Ragle CA: Canine pyometra: an update on pathogenesis and treatment. Compend Contin Educ Pract Vet 25:602–612, 2003
29. Fukuda S: Incidence of pyometra in colony-raised beagle dogs. Exp Anim 50:325–329, 2001
30. Von Berky AG, Townsend WL: The relationship between the prevalence of uterine lesions and the use of medroxyprogesterone acetate for canine population control. Aust Vet J 70:249–250, 1993
31. Nelson RW, Feldman EC: Pyometra. Vet Clin North Am Small Anim Pract 16:561–576, 1986
32. Klein MK: Tumors of the female reproductive system, in Withrow SJ (eds): Small Animal Clinical Oncology (ed 2). Philadelphia, PA, Saunders, 1996, pp 351
33. Brodey RS: Neoplasms of the canine uterus, vagina and vulva: a clinicopathologic survey of 90 cases. J Am Vet Med Assoc 151:1294–1307, 1967
34. Vos JH: Uterine and cervical carcinomas in five dogs. J Vet Med 35:385–390, 1980
35. Ogilvie GK, Moore AS: Tumors of the reproductive system, in Managing the veterinary cancer patient. New Jersey, Veterinary Learning Systems Co., Inc, 1995, pp 419–420
36. Holt PE, Thrusfield MV: Association in bitches between breed, size, neutering and docking, and acquired urinary incontinence due to incompetence of the urethral sphincter mechanism. Vet Rec 133:177–180, 1993
37. Thrusfield MV: Associations between urinary incontinence and spaying in bitches. Vet Rec 116:695, 1985
38. Arnold S: Harninkontinenz bei kastrierten Hu¨ndinnen. Teil 1: Bedeutung, Klinik und A¨tiopathogenese. Schweiz Arch Tierheilkd 139:271–276, 1997
39. Nickel RF, Van Wees AM, Van Den Brom WE, et al: Changes in urethral closure and bladder storage function in young female dogs caused by prepubertal events, the estrous cycle, and neutering, PhD Dissertation, RF Nickel, RU Utrecht, Chapter 7, pp. 87–110.
40. Janssens LA, Peeters S: Comparison between stress incontinence in women and sphincter mechanism incompetence in the female dog. Vet Rec 141:620–625, 1997
White RN: Urethropexy for the management of urethral sphincter mechanism incompetence in the bitch. J Small Anim Pract 42:481–486 42. Blendinger C, Blendinger K, Bostedt H: Die Harninkontinenz nach Kastration bei der Hu¨ndin. 1. Mitteilung: entstehung, Ha¨ufigkeit und Disposition. Tiera¨rztl Prax Ausg K Klientiere Heimtiere 23:291–299, 1995 43. Spain CV, Scarlett JM, Houpt KA: Long-term risks and benefits of early-age gonadectomy in dogs. J Am Vet Med Assoc 224:380–387, 2004 44. Ruckstuhl B: Die incontinentia urinae bei der Hu¨ndin als Spa¨tfolge der Kastration. Schweiz Arch Tierheilkd 120:143–148, 1978 45. Arnold S, Arnold P, Hubler M, et al: Incontinentia Urinae bei der kastrierten Hu¨ndin: ha¨ufigkeit und Rassedisposition. Schweiz Arch Tierheilkd 131:259–263, 1989
46. Salmeri KR, Olson PN, Bloomberg MS: Elective gonadectomy in dogs: a review. J Am Vet Med Assoc 198:1183– 1192, 1991
47. Edney AT, Smith PM: Study of obesity in dogs visiting veterinary practices in the United Kingdom. Vet Rec 118:391– 396, 1986
48. Le Roux PH: Thyroid status, oestradiol level, work performance and body mass of ovariectomized bitches and bitches bearing ovarian autotransplants in the stomach wall. J S Afr Vet Assoc 54:115, 1983
49. Houpt KA, Hintz HF: Obesity in dogs. Canine Pract 5:54–58, 1978
50. Houpt KA, Coren B, Hintz HF, et al: Effect of sex and reproductive status on sucrose preference, food intake, and body weight of dogs. J Am Vet Med Assoc 174:1083–1085, 1979
From the Department of Clinical Sciences of Companion Animals, Faculty of Veterinary Medicine, Utrecht University, Utrecht, The Netherlands.
Address reprint requests to Bart Van Goethem, DVM, Spoorweglaan 38A, 9140 Temse, Belgium. E-mail: bart.vangoethem@tiscali.be.
Submitted April 2005; Accepted June 2005
© Copyright 2006 by The American College of Veterinary Surgeons
0161-3499/04
doi:10.1111/j.1532-950X.2006.00124.x
 .
.